Proprietary hardware and software algorithms enable best-in-class performance, while simple setup and reliable operation offer an unrivaled user experience.

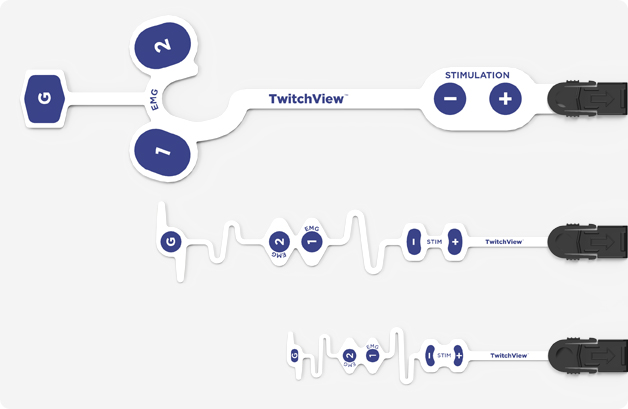
Adult and pediatric electrodes can be rapidly placed on either the hand or foot.
Electromyography (EMG) based measurements require no motion and can be utilized on tucked arms.
One button startup and AutoPTC enables continuous monitoring across all levels of neuromuscular blockade (TOF Ratio, TOF Count, Post-Tetanic Count).
Integration with electronic medical records (EMRs) eliminates manual charting.

We understand that new technology adoption requires planning, collaboration and education. Blink DC has created a suite of tools to facilitate success, and we will partner with your institution to ensure an effective TwitchView implementation and ongoing use.


We understand that new technology adoption requires planning, collaboration and education. Blink DC has created a suite of tools to facilitate success, and we will partner with your institution to ensure an effective TwitchView implementation and ongoing use
Attending Anesthesiologist, University of Washington
Beyond usability, TwitchView is the ONLY quantitative neuromuscular monitor clinically validated as accurate and interchangeable with gold-standard mechanomyography (MMG). When clinical decisions are based on monitor data—accuracy matters. TwitchView has been validated in multiple independent studies and proven accurate from deep blockade to recovery.

"The TOF ratio measured with TwitchView, resembled gold-standard mechanomyography (MMG)4"

"Electromyography (EMG) with TwitchView and mechanomyography (MMG) most closely correlated with the palpated count3"

"Reversal with Sugammadex was deemed unnecessary in all cases managed clinically with the TwitchView Train of Four monitor.1"
"Using TwitchView, we eliminated the occurrence of residual neuromuscular blockade and utilized Sugammadex in less than 50% of patients2"
Attending Anesthesiologist, Philadelphia Academic Institution
In addition to real-time measurements, TwitchView displays the patient's level of blockade and recovery on a trend plot.The trend plot enables clinicians to visualize how neuromuscular blocking agents affect each patient differently, often leading to less overall drug use and more reversal options. Most importantly, adequacy of reversal is confirmed by a TOF ratio > 90% prior to extubation, which eliminates the possibility of residual neuromuscular blockade (RNMB) and supports conservative reversal choices.

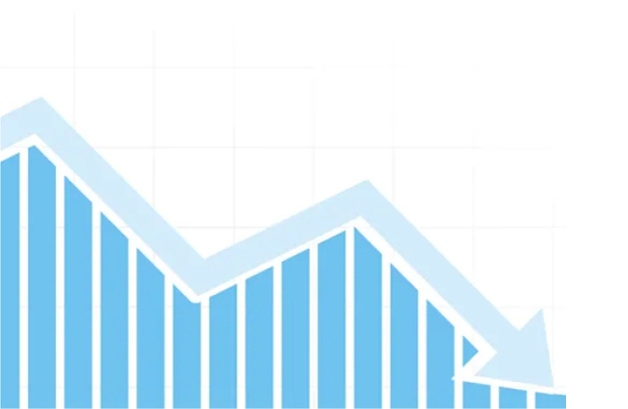

"The maximum potential cost savings for Temple University Hospital derived from eliminating post operative pulmonary complications associated with residual neuromuscular blockade would be roughly $7 million dollars annually. This compares very favorably with an annual cost of implementing universal [TwitchView] quantitative train of four monitoring of $162,000."1
- Dr. Gordon Morewood, Chair and Professor of Anesthesiology at Temple University
Leading hospitals are already benefitting from TwitchView utilization.
We understand that new technology adoption requires planning, collaboration and education.
Blink DC has created a suite of tools to facilitate success, and we will partner with your institution to ensure an effective TwitchView implementation and ongoing use.
References: 1. Ly N, Edwards LA, Morewood G. The influence of EMG-based quantitative TOF monitoring on clinical decision making. Paper presented at: Postgraduate Assembly in Anesthesiology; December 13-17, 2019; New York, NY. 2. Thilen SR, Sherpa J, Treggiari MM, James A, Cain KC, Bhananker SM. Best Management of Muscle Relaxation with Rocuronium Using Objective Monitoring and Reversal with Neostigmine or Sugammadex. Oral presentation Feb 28, 2020, Whistler Anesthesia Summit, Whistler, BC, Canada. 3. Bowdle A, Bussey L, Michaelsen K. Counting train-of-four twitch response: comparison of palpation to mechanomyography, acceleromyography, and electromyography. Br J Anaesth. 2020;124(6):712-717. 4. Bowdle A, Bussey L, Michaelsen K, et al. A comparison of a prototype electromyograph vs. a mechanomyograph and an acceleromygraph for assessment of neuromuscular blockade. Anesthesia. 2020;75(2):187-195.